53yr male with swelling of face
A 53-year-old male, a Hotel owner and chief by occupation,
The patient presented to the hospital with chief complaints of
Swelling of both Legs since 10 days
Swelling of face since 7 days
- yellowish discolouration of urine
PAST HISTORY
PERSONAL HISTORY
GENERAL EXAMINATION
Pallor- present
Icterus-present
Cyanosis-absent
Clubbing-present
Lymphadenopathy-absent
Edema -present b/l pitting type .
Temperature-97.6'f
Pulse rate -90bpm.
Bp-150/80mm hg
RR-17cpm
Spo2-99% .
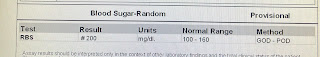
grbs-110mg/
Abdomen examination
INSPECTION:-
Shape of abdomen -distended
Umbilicus-inverted.
No scars ,sinuses,straie
No visible pulsations & visible peristalsis.
Moments of all 4quadrants moving equally with respiration
Shifting dullness-+
No signs of fluid thrill.
CVS:-
S1,S2heard ,no murmurs.
CNS :-
Higher motor functions - intact
Cranial nerves - intact
Sensory system - intact
Chest moments -normal
Bae-+
13.06.2023
Ascitic Fluid
Volume-3ml
Colour-clear
Rbc-nil
Tc-50
Dc-100
Others nil
ENDOSCOPY FINDINGS:
Esophagus : Grade -1 Esophageal varices (2 columns)
Stomach : Severe PHG ( portal hypertension gastropathy)
Duodenum: D1 D2 normal
Impression : Severe PHG with Grade -1 Esophageal varices
PROVISIONAL DIAGNOSIS:
DECOMPENSATED CHRONIC LIVER DISEASE WITH PORTAL HYPERTENSION (SPLENOMEGALY,MODERATE ASCITIS) WITH THROMBOCYTOPENIA SECONDARY TO CLD ? B12 DEFICIENCY WITH ALCOHOL WITHDRAWAL STATE.
Treatment:
Fluid restriction <2l /day
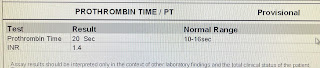
Injection - vitk IV/ OD ( 1Amp in 100 ml NS)
CAP-evion 400mg PO/OD
Tab- Benfothiamine 100mg PO/ TID
Tab UDILIV 300mg PO/BD
Tab Lorazepam 2mg 1-1-2
Tab Baclofen 20mg OD(HS)
Tab Aldactone 50mg OD 2pm
Syrup-lactulose 15ml / PO/ BD
Salt restriction <2l/day
Protein rich diet (2egg white/day)



































Comments
Post a Comment